This webinar focused on the development and deployment of patient-centered outcome measures (PCOMs) for research and care, highlighting the importance of integrating patients’ voices into the research process. Unlike traditional patient-reported outcomes (PROs), which often focus solely on symptoms, PCOMs take a broader approach by incorporating what matters most to patients in terms of care and daily life. The webinar speakers (listed above) shared their experiences developing patient-centered outcome measures in the rare disease and obesity spaces.
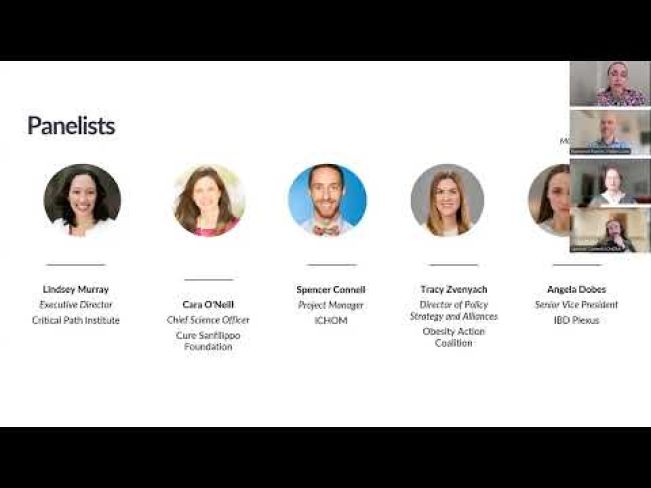
Moderator
Angela Dobes, MPH
Senior Vice President, IBD Plexus, Crohn’s and Colitis Foundation
Speakers
Lindsey Murray, PhD, MPH
Executive Director, Critical Path Institute
Cara O’Neill, MD, FAAP
Chief Science Officer, Cure Sanfilippo Foundation
Spencer Connell, MS, DAT
Project Manager, ICHOM
Tracy Zvenyach, PhD, MS, RN
Director of Policy Strategy and Alliances, Obesity Action Coalition
Patient-Centered Outcome Measures (PCOMs) in Research and Care
Patient-centered outcome measures go beyond traditional clinical metrics by focusing on what truly improves patients' quality of life and daily function. Incorporating these outcomes requires input from patients, caregivers, and patient advocacy groups to ensure that research and care processes address patients' needs. By utilizing PCOMs, clinical research and trials can focus on additional outcomes that matter to patients, such as daily living improvements, in addition to disease progression or symptom relief.
Developing PCOMs for Rare Diseases
Lindsey Murray, PhD, MPH, of the Critical Path Institute spoke about the challenges in rare disease research, particularly the scarcity of standardized outcome measures. She explained how the Rare Disease Clinical Outcome Assessment (COA) Consortium has worked to create tools for rare diseases that address daily function and pain, areas that are often of critical importance to patients but not well-represented in traditional research. The consortium has already developed measures for gross motor function, fine motor function, communication, and self-care, and is now expanding into areas such as pain and sleep disturbance.
Strategies for Implementing PCOMs
- Use of Existing Measures: Whenever possible, organizations are encouraged to adopt or modify existing outcome measures, particularly for complex conditions such as rare diseases. This can save time and resources while ensuring that research stays on track.
- Collaborative Development: Developing PCOMs should involve close collaboration between patient advocacy groups, researchers, and regulatory bodies. Including patients in the decision-making process helps ensure that the measures chosen reflect their real-world experiences and priorities.
- Tailoring to Specific Conditions: Adapting tools to fit the specific needs of different patient populations is critical. For example, in rare diseases where there may be significant variability between patients, PCOMs must be designed or adjusted to capture important outcomes—such as physical function or quality of life—that may vary widely.
Challenges in Aligning Stakeholders
One of the key challenges in developing PCOMs is aligning the interests of different stakeholders, such as regulators, sponsors, patients, and health-care providers:
- Differing Priorities: While short-term, measurable outcomes are often prioritized in clinical trials to show efficacy quickly, these may not align with patient priorities, which often focus on long-term improvements in quality of life. Striking a balance between these needs is a recurring challenge.
- Resource Barriers for Small Organizations: Smaller patient advocacy organizations may face significant resource constraints when developing and validating PCOMs. Partnering with experienced research teams can help overcome these barriers.
- Cultural and Global Variations: When implementing PCOMs across different countries or regions, organizations must ensure that the outcome measures are culturally relevant and validated for use in diverse settings. This often requires working with translation and validation experts to maintain the integrity of the measures across various cultural contexts.
Lessons Learned
- Patient Involvement Is Crucial: Direct patient involvement from the start of the process ensures that the outcome measures are relevant and reflect real-world needs. This approach leads to the selection of outcomes that truly impact patients’ quality of life.
- Flexibility in Tool Use: While existing tools are useful, there may be cases where creating new tools is necessary. For example, new outcome measures may need to be developed in rare diseases, where current tools may not adequately capture patient experiences.
Future Trends
Emerging trends in the use of PCOMs include:
- Long-Term Use in Gene Therapy and Obesity Management: As new therapies, including gene therapies and obesity management treatments, are developed, patient-centered outcome measures become essential for tracking long-term benefits. These therapies often take years to show full effects, making ongoing monitoring through PCOMs crucial.
- Regulatory Adoption: Regulatory agencies are increasingly incorporating PCOMs in their assessments of clinical trials and new treatments. This shift is encouraging researchers and pharmaceutical companies to develop and submit PCOMs to demonstrate the broader impact of their therapies on patients’ lives.
Conclusion
Providers, patient organizations, and pharmaceutical and biotech organizations are all encouraged to prioritize PCOMs in their research and clinical efforts. By focusing on outcomes that are important to patients and working collaboratively with stakeholders, it is possible to create measures that lead to meaningful improvements in both research outcomes and patient care.
For additional resources, please visit some shared by speakers, including the Rare Disease COA Resource and ICHOM sets, which include open-access flyers, reference guides, and scientific publications for anyone to utilize and replicate.

